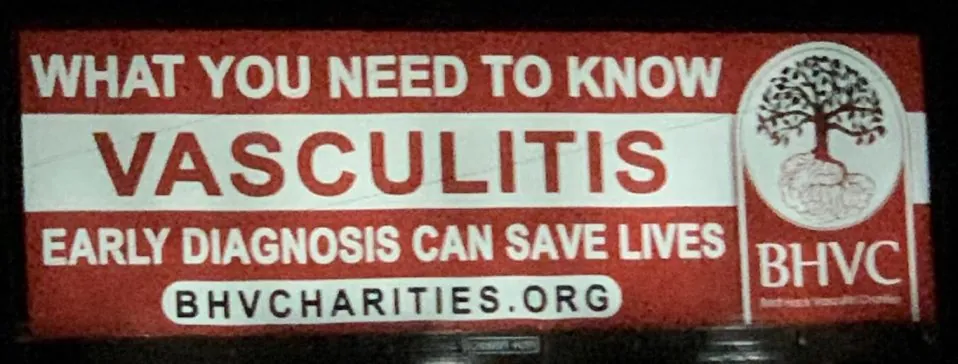
Explore the tool and find trusted vasculitis care wherever you live.
We are you. We are patients with vasculitis, care partners, friends, family, physicians, and researchers advocating for early diagnosis, better treatments, and improving quality of life for people with vasculitis. Explore. Learn. Download Resources. Join a Support Group.
Vasculitis Types
About Anti-GBM Disease
Last Updated on February 5, 2024
Anti-GBM (anti-glomerular basement membrane) disease is a rare, but serious autoimmune disease that causes inflammation of the small vessels in the kidneys and lungs. In this disease, the immune system mistakenly makes “anti-GBM antibodies,” which attack the lungs and kidneys, causing bleeding and damage to those organs. The disease can progress rapidly to life-threatening lung and kidney failure, so early diagnosis and treatment are vital. Smoking and exposure to certain chemicals may be among the triggers for this disease.

Quick Facts

2 Cases per million worldwide

Number of US cases unknown

Typically seen in two age groups: 20-30 and 60 or older

Rare in children

More common in males

More common in Caucasians of European descent
Anti-GBM (anti-glomerular basement membrane) disease is a rare, but serious autoimmune disease that causes inflammation of the small vessels in the kidneys and lungs. In this disease, the immune system mistakenly makes “anti-GBM antibodies,” which attack the lungs and kidneys, causing bleeding and damage to those organs. The disease can progress rapidly to life-threatening lung and kidney failure, so early diagnosis and treatment are vital. Smoking and exposure to certain chemicals may be among the triggers for this disease.
The term Goodpasture’s syndrome has been used in the past, when both lungs and kidneys are affected in the presence of the anti-GBM antibodies, but the preferred name for the disease now, is anti-GBM disease. Anti-GBM disease may affect only the kidneys; lungs are involved in about 50% of patients. This disease may come on suddenly, with early symptoms of fatigue, nausea, pale skin, and shortness of breath. As the disease progresses, patients may cough up blood, have dark urine, leg swelling, and chest pain, among other signs and symptoms.
Treatment for anti-GBM disease typically includes glucocorticoids and plasma exchange procedure (plasmapheresis), which removes the harmful antibodies from the blood. Ongoing medical care is essential to monitor disease progression and medication side effects.
The cause of anti-GBM disease is not fully understood. It is classified as an autoimmune disorder—a disease that occurs when the body’s natural defense system mistakenly attacks healthy tissue. Researchers believe a combination of factors may trigger anti-GBM disease including genetics, respiratory infections, exposure to certain chemicals (hydrocarbon fumes, metallic dust), use of certain drugs such cocaine, and tobacco smoking.
Anti-GBM disease is very rare, with an estimated incidence of about 10 cases per million in hospitalized patients. It typically affects people in two age groups – young people aged 20 to 30, and people 60 and older. It is most common among young Caucasian men and is rare in children.
Early symptoms include general body aches and pains; fatigue, weakness or lethargy, pale skin, nausea and lack of appetite, cough, and shortness of breath. Anti-GBM disease can progress rapidly to the lungs and kidneys, with the following symptoms:
- Persistent dry cough
- Coughing up blood (bleeding in the lungs can cause respiratory failure, so seek immediate medical attention if you are coughing up blood.)
- Bloody (dark) and/or foamy urine
- Difficult urination
- Swelling in the legs, hands or feet
- Chest pain
Both kidney and lung failure are life-threatening complications of anti-GBM disease. Kidney failure is the most serious complication and may require kidney dialysis or even kidney transplant. The disease can also cause life-threatening bleeding in the lungs; however, early diagnosis and treatment can help prevent long-term lung damage.
There is no single test to diagnose anti-GBM disease. Your doctor will consider several factors including a detailed medical history, physical examination, laboratory tests, and specialized imaging studies. Diagnosis is usually confirmed by the presence of anti-GBM antibodies in a blood test, and through a kidney biopsy—the gold standard for diagnosis of this disease.
Diagnosis involves ruling out diseases that cause similar symptoms including other forms of vasculitis. Depending on organs affected, the following diagnostic tests may be ordered:
- Blood tests: Detecting the presence of anti-GBM antibodies in the bloodstream is key to confirming the diagnosis.
- Urinalysis: Excessive protein or presence of red blood cells may indicate kidney inflammation.
- Imaging studies: Chest X-ray or computed tomography (CT) scan may reveal bleeding or lung changes/damage.
- Tissue biopsy: This surgical procedure removes a small tissue sample from the kidneys or lungs, which is examined under a microscope for signs of inflammation or tissue damage.
Treatment for anti-GBM disease is aimed at reducing inflammation, halting further antibody production, and removing anti-GBM antibodies from the bloodstream. Treatment usually requires plasmapheresis (plasma exchange) in which the liquid part of the blood (plasma) is removed, filtered of the harmful anti-GBM antibodies, and then returned to the body. This procedure is typically done for about two weeks. Medications include glucocorticoids such as prednisone, in combination with the immunosuppressive medication cyclophosphamide. Intravenous glucocorticoids may be required to control bleeding in the lungs.
If the disease leads to kidney failure, kidney dialysis or transplant will likely be required.
The medications used to treat anti-GBM disease have potentially serious side effects such as:
- Lowering your body’s ability to fight infection
- Potential bone loss (osteoporosis), among others
Therefore, it’s important to see your doctor for regular checkups. Medications may be prescribed to offset side effects. Infection prevention is also very important. Talk to your doctor about getting vaccines (e.g., flu shot, pneumonia and/or shingles vaccination), which can reduce your risk of infection.
Relapses are rare with anti-GBM disease. However, if your symptoms return or you develop new ones, report them to your doctor as soon as possible.
Effective treatment of anti-GBM disease may require a team of medical providers and specialists. In addition to your primary care provider, you may need to see the following specialists:
- Rheumatologist (joints, muscles, immune system)
- Nephrologist (kidneys)
- Pulmonologist (lungs) or others as needed
The best way to manage your disease is to actively partner with your health care providers. Get to know the members of the health care team. It may be helpful to keep a health care journal to track your medications, symptoms, test results and notes from doctor appointments in one place. To get the most out of your doctor visits, make a list of questions beforehand and bring along a supportive friend or family member if necessary to provide a second set of ears and take notes.
Remember, it’s up to you to be your own advocate. If you have concerns about your treatment plan, be sure to speak with your medical team. It is always your right to seek a second opinion.
Living with a chronic disease can be challenging at times. Fatigue, pain, emotional stress, and medication side effects can take a toll on your sense of well-being, affecting relationships, work, and other aspects of your daily life. Sharing your experience with family and friends, connecting with others through a support group, or talking with a mental health professional can help.
Anti-GBM disease is often severe and requires prompt and aggressive treatment to avoid life-threatening lung and kidney failure. The outlook especially depends on the disease’s effect on the kidneys. Patients have the best outcome when treatment is started before kidney dialysis is required. Relapse is rare with this disease, and it typically doesn’t require long-term treatment. Avoiding cigarette smoke and inhaled toxins may improve a patient’s outlook.
Anti-GBM Videos
Preventing progressive chronic kidney disease in vasculitis
Managing Chronic Pain in Vasculitis: Tools, Treatments, and Hope 2026