A Journey Through the Fog: Eric Trainor’s Battle with CNS Vasculitis
 For 56-year-old Eric Trainor of Wonder Lake, Illinois, a man who describes himself as caring and sensitive, and who has proudly maintained 24 years of sobriety, August 1, 2024, began like any other day. Married to his wife, Karen, for 19 years, and a devoted owner of two dogs, Tigger and Ember, Eric’s life took an abrupt turn when a sudden and alarming change in his vision prompted immediate action. “I asked a coworker to call 911 thinking I was having a stroke,” he recalled, describing the moment partial vision loss struck both eyes.
For 56-year-old Eric Trainor of Wonder Lake, Illinois, a man who describes himself as caring and sensitive, and who has proudly maintained 24 years of sobriety, August 1, 2024, began like any other day. Married to his wife, Karen, for 19 years, and a devoted owner of two dogs, Tigger and Ember, Eric’s life took an abrupt turn when a sudden and alarming change in his vision prompted immediate action. “I asked a coworker to call 911 thinking I was having a stroke,” he recalled, describing the moment partial vision loss struck both eyes.
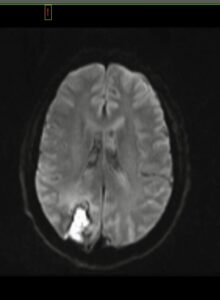
The swift response of emergency services led to stroke protocols and a subsequent CAT scan, which unveiled something unexpected: a mass in the back of his brain. A biopsy followed the next day, along with high doses of steroids to combat the swelling. Eric believes he started taking prednisone that very day, or within a couple of days. After a week of recovery at Northwestern Central DuPage Hospital, Eric was sent home with an unspoken diagnosis of brain cancer.
However, the respite was short-lived. “I was home for a day and a half when the neurologist called, on a Sunday, instructing me to return to the hospital as soon as possible and go to the ER,” Eric explained. The news was significant: It wasn’t cancer, but central nervous system (CNS) vasculitis. Eric’s brain biopsy and bloodwork were tested for everything imaginable, including cancer, infectious diseases, and even fungus. It was the lab’s inability to culture anything from the biopsy along with certain markers in his bloodwork that led to the CNS vasculitis diagnosis.
Escalating Symptoms and a Critical Turning Point
Another week of high-dose IV steroids aimed at reducing inflammation in his brain and at the site of the vasculitis followed. Upon discharge, the instructions were clear: Connect with a neurologist specializing in autoimmune diseases. Living 60 miles outside of Chicago, Eric was lucky to find exactly the doctor he needed. Dr. Kelly Donohue is a neuro critical care specialist at Northwestern Medicine Regional Medical Group in Chicago’s northwest suburbs.
From this point on, Eric’s memories become fuzzy. His wife, Karen, has filled in the subsequent timeline, painting a picture of a challenging period, leading to another hospital readmission in October 2024. It was then that unsettling symptoms emerged. “I started having visual and auditory illusions—things I saw and heard but knew weren’t real,” Eric said.
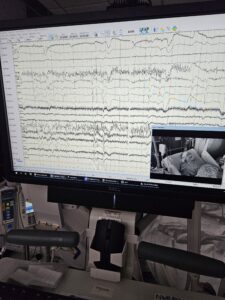
This time, at Northwestern Hospital in McHenry, Eric’s condition escalated. “I became psychotic, with true hallucinations and altered reality.” The ICU neurology team, including nurses trained in the care of neurology patients, intensified steroid treatment, but instead of improvement, Eric’s condition worsened. Days of EEGs revealed a concerning pattern: near-constant mini-strokes and seizure activity. The ICU doctor was a neurologist who shifted the medical team’s approach, introduced a variety of anti-seizure medications and intravenous immunoglobulin (IVIG). Gradually, Eric’s brain began to calm down. “It was a very long 16 days before I was discharged on three anti-seizure medications,” he noted.
Treatment, Therapy, and Lingering Damage
The road to recovery continued with a significant steroid regimen. “I have been on 60 mg of prednisone a day since September,” Eric shared. While he said that much of what he experiences could be attributed to either the illness or the medication, he’s certain of one side effect—significant weight gain due to the prednisone. Despite the ordeal, he experienced some progress after his second hospitalization.
Even so, Eric endured three months of physical, occupational, and speech (cognitive) therapy, yet the neurological damage left lasting effects. “I lost the field of vision on my left side in both eyes; the cut is different in each eye,” Eric explained. “I have issues with double vision and my eyes getting tired quickly when looking at anything small, like a phone, laptop, or labels.” The cognitive impairment is equally challenging, causing him to lose focus and sometimes forget what he’s saying mid-sentence. Tasks as simple as typing become difficult and even spelling, he admitted, is a struggle. “I still have to guess at how to spell vasculitis,” he shared, highlighting the persistent impact of an illness he had never heard of before his diagnosis.
The neurological damage also led to a new diagnosis for Eric. “Because of all the damage my brain suffered, I’ve been diagnosed with epilepsy and now have an epileptologist on my team.” The implications of epilepsy weigh heavily on him. “The epilepsy scares me that I might have a seizure or that I might be having focal seizures and not know it,” he confided, adding that the anti-seizure drugs make him tired and spacey. The consequences of both conditions have been life-altering. “I’m on long-term disability now because I can’t drive and I still have some cognitive problems that affect my ability to work. Everything is different. I went from full-time employment, fishing, and working on home improvement projects, to doing maybe a couple small exercises I learned in PT/OT/speech therapy and being done for the day.”
Eric recounted learning to take his time, making multiple trips in the kitchen to ensure everything is put away, and only cooking with a timer when alone, still worrying about leaving utensils in the microwave. He’s learned that stress only makes it worse. Adding a remarkable detail from his initial surgery, Eric said, “Fun fact, when they did the biopsy and took the piece of skull off, my brain bulged out due to so much swelling.”

Glimmers of Progress and Hope
Now, months later, there’s a glimmer of hope and evidence of Eric’s resilience. At the time of this interview, Eric had recently finished seven months of chemotherapy, and the MRI conducted shortly afterward showed no new abnormalities, confirming the treatment’s effectiveness. “EEG didn’t show any signs of seizure or stroke activity in the brain. Next step is to taper off prednisone (hopefully).”
The invisible toll on Eric’s mental and emotional well-being has been substantial. He has been diagnosed with depression, anxiety, and PTSD. To cope, he takes an antidepressant, attends weekly sessions with a psychologist, and finds solace in his AA group. “My wife is my rock! Top of my gratitude list,” Eric declared, emphasizing the critical role Karen plays. He noted that most days he can remain positive, but when he feels “down, lost or freaked out,” a hug from Karen often helps. His dogs, Tigger and Ember, also possess an uncanny ability to sense his struggles, often comforting him or prompting him to go outside and play. Eric also finds support through family, friends, and the Inspire website, highlighting a robust support system.
Eric has been to a neuro ophthalmologist to monitor the health of his eyes and optic nerves. He will be starting visual rehab soon with a low vision specialist to try to improve his double vision, though there’s nothing to be done to restore the vision he has lost.
A Story of Endurance and Advocacy
Eric’s journey through the complexities of CNS vasculitis highlights the unpredictable nature of autoimmune diseases and the difficult path to recovery. His story is a powerful reminder of the importance of prompt medical attention, the challenges of diagnosis, and the long-term impact such conditions can have on a person’s life. For Eric, the phrase “one day at a time” has taken on a more profound meaning than even during his journey to sobriety.
What keeps him going are his wife, dogs, and family, along with the hope of eventually being able to fish or golf again, and the goal of tapering off prednisone. He also lives by the mantra, “I love you, God must think you’re a badass.”
Eric’s advice to anyone newly diagnosed with vasculitis is clear: “Ask every question that comes into your mind, advocate for yourself and/or have family and friends advocate for you.” His determination and the support of his loved ones continue to be vital as he navigates the next chapter of his recovery.
