“Onwards and Upwards” — Samantha Feeney’s Journey to a Vasculitis Diagnosis

Samantha lives in Northamptonshire, England, with her husband Adam, whom she has been married to for 30 years. At 57, she describes herself as “outgoing, positive, artistic, and creative.” She is a mother to her daughter Alessandra (34) and a proud grandmother to four grandchildren — James and Atlas (9), Oberon (7), and baby Olive, six months old. But in recent years, her life has been reshaped by granulomatosis with polyangiitis (GPA).
Treatment Began Aggressively
Treatment started with prednisolone and avacopan, followed by nine cyclophosphamide infusions. Over time, medications were repeatedly adjusted due to flares and side effects, including methotrexate, mycophenolate, rituximab, and eventually leflunomide. Steroid-related bone loss led to fractured vertebrae and ongoing osteoporosis treatment.
“The nurses who look after me on infusion day – Comfort Adedoyin Dawodu, RDU Manager, and Ann Barcelona and Karolina Karwala (specialist nurses) – listen and make me feel like I have their full attention,” Samantha said. “I never feel like a number or that I’m just being processed. They are awesome.”
For decades, Samantha had barely taken so much as a painkiller. “I was proud of that,” she said. “Now I take around 20 tablets a day, plus monthly injections, and infusions. That was one of the hardest changes to accept.”
Side effects have been hard to untangle. “It’s impossible to say what caused what,” she said. “Steroids gave me moon face and bone issues. I feel spaced out, tired, and achy — but I’m better than I was, and I’m grateful for that.”
Living with Vasculitis
Daily life with vasculitis remains challenging. Samantha is now deaf in both ears and relies on hearing aids. For nearly two years, she lost her sense of taste and smell. Though her vision is stable, she often feels disconnected. “With the hearing loss, it’s like being in a cloud — isolated from the real world.”
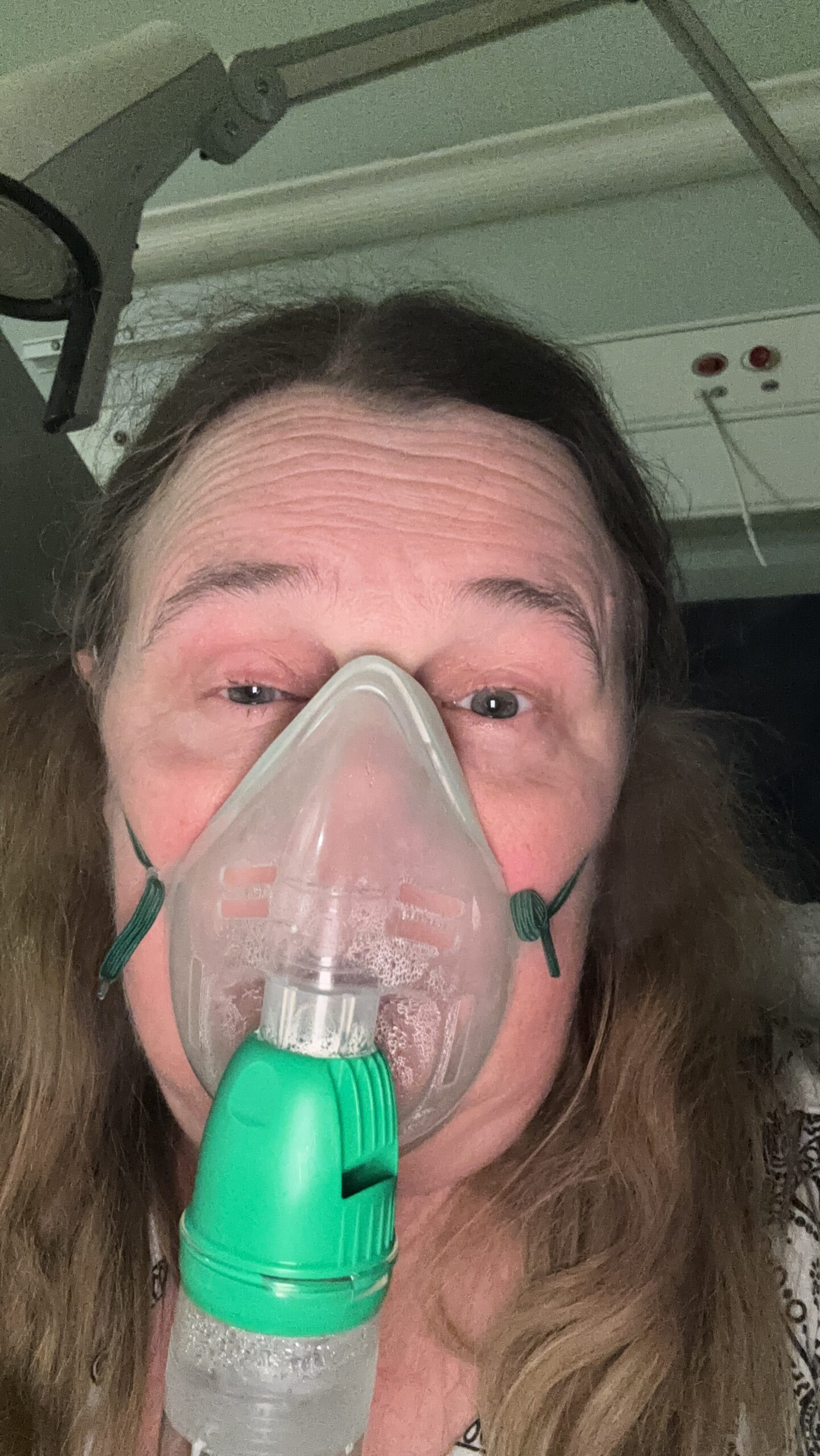
Fatigue, pain, breathing issues, and reduced mobility have taken their toll. Recognizing the impact on her mental health, Samantha made a decisive change. “Not wanting to be defeated, I bought a mobility scooter,” she said. “Now I can join my husband on dog walks and go to the shops. It’s brilliant.”
She took early retirement at 55, ending a career she loved as a bank trainer. “The hearing loss and brain fog made it impossible.”
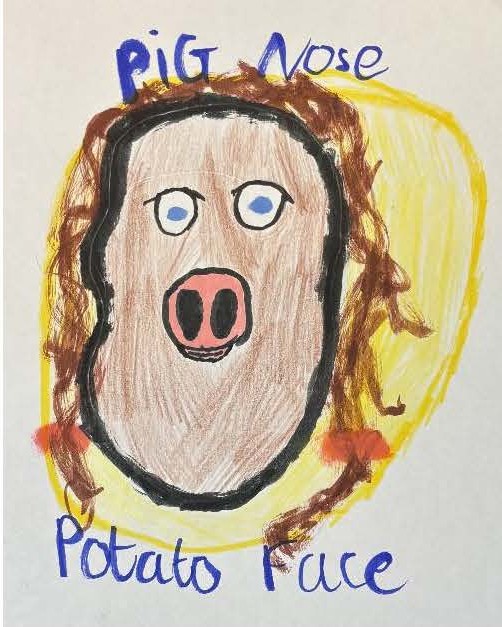
Emotionally, the journey has been just as hard. Samantha speaks openly about depression, grief for her former self, and visible changes caused by both disease and treatment. “I look so different… sometimes I hide, but mostly I front it out.” Her humor remains intact. “Before you ask, I don’t take cocaine and I don’t have syphilis,” she joked — pre-empting questions about her collapsed nose.
Her mantra, “onwards and upwards,” guides her through setbacks. “First, I get angry, then sad — and then I pick myself up and try to think positive. I’m not giving up.”
Support has been crucial. “My husband Adam is my rock,” she said. Her daughter, grandchildren, a dedicated GP nurse, Lauren Bailey, and support from Vasculitis UK, the Vasculitis Foundation, and online communities have helped her through.
Vasculitis has changed how Samantha sees the world. “I don’t worry about the small stuff anymore,” she said. “Family and experiences are what matter.”
Looking ahead, she hopes for camping holidays, time with her grandchildren, getting back to lawn bowls, and eventually nose reconstruction surgery. Until then, she holds onto hope, humor, and perspective. “I’m thinking about sharing a VLOG online about day-to-day life with GPA and my adventures on ‘Mario,’ my mobility scooter,” Samantha said. “That’s a work in progress.”
“I often refer to myself as ‘Pig Nose, Potato Face,’” Samantha said with a laugh — a phrase she’s considering using for the future VLOG once she plucks up the courage. Her grandson Atlas even drew her a picture.
Her advice to others newly diagnosed is simple: “Everyone’s journey is different. Try to stay positive. Have faith — the science is moving fast. Stay in touch with your rheumatologist. REST.”
And always, onwards and upwards.
